Falling over or feeling less steady than before? Fearful of falling? Then this article is for you. Read on to learn more about what you can do.
The Problem of Falls
Studies have shown that 1 in 3 seniors above 65 years old has had a fall in the past year. This statistic increases to 1 in 2 above the age of 85.
1 in 10 of these falls result in a serious injury such as a hip fracture. 1 in 2 of these seniors may never regain their mobility and independence.
Why do Seniors tend to Fall?
Seniors tend to fall more frequently due to a combination of physical, health, and environmental factors. Falls also tend result in more serious injuries including fractures and long hospitalisations.
Here are some key reasons:
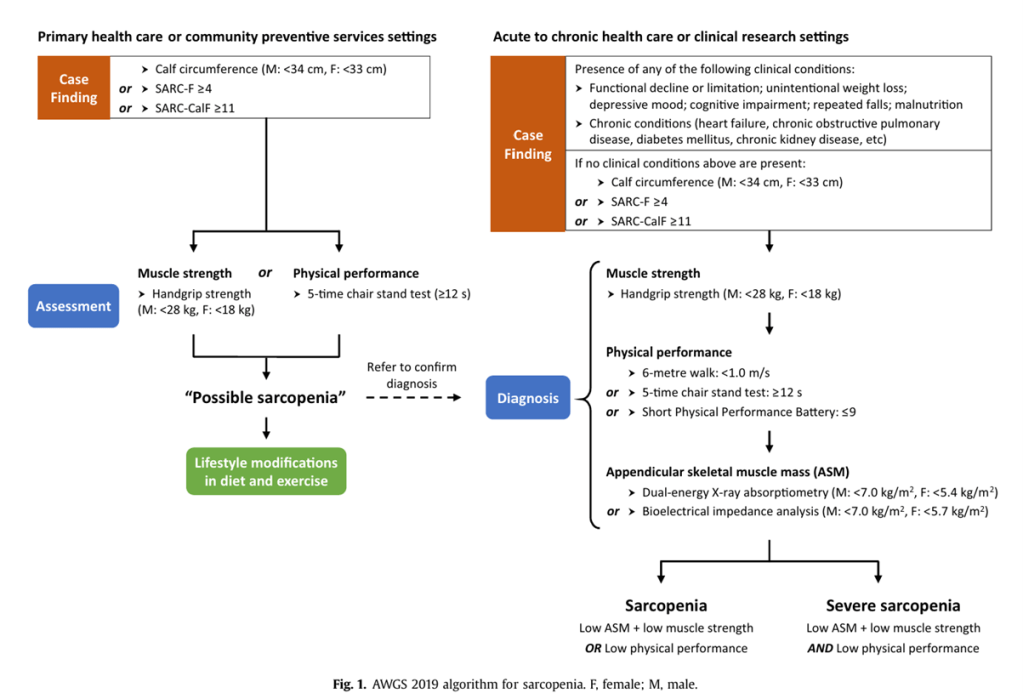
1. Decline in Muscle Strength (Sarcopenia):
As people age, they often lose muscle mass and strength, a condition called sarcopenia. Weaker muscles make it harder to maintain balance, and an older person may be more prone to falling when they lose their footing or need to react quickly to avoid an obstacle.
2. Decreased Balance and Coordination:
Ageing affects the nervous system, which controls balance and coordination. Older adults may have slower reaction times, difficulty adjusting to shifts in position, or less stability when standing or walking, making them more vulnerable to falls.
3. Vision Problems:
As we age, our vision can deteriorate due to conditions like cataracts or age-related macular degeneration. Poor vision can make it harder to see obstacles, stairs, or uneven surfaces, increasing the risk of tripping or stumbling.
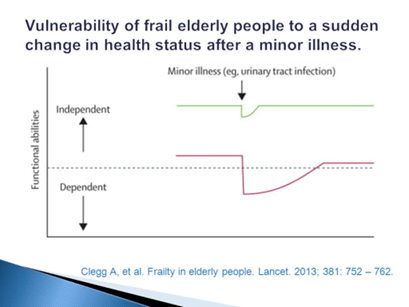
4. Chronic Health Conditions:
Certain conditions common in older adults—such as arthritis, diabetes, Parkinson’s disease, and heart disease—can affect mobility and increase the risk of falling. For example, Parkinson’s disease can cause tremors and difficulty walking, while arthritis can make it painful to move properly.
5. Medication Side Effects:
Many older adults take multiple medications, some of which can cause dizziness, low blood pressure, or drowsiness. These side effects increase the likelihood of falls. For example, medications for blood pressure, antidepressants, or sedatives can make individuals feel lightheaded or less stable.
6. Osteoporosis and Fragile Bones:
Older adults, particularly women, are at greater risk of osteoporosis, which weakens bones and makes them more likely to fracture if a fall occurs. A fall that might only cause a bruise in a younger person can result in a serious bone injury in an older person.
7. Reduced Physical Activity:
Lack of regular exercise can contribute to muscle weakness, poor balance, and slower reflexes. Many older adults become less active due to health concerns or fear of falling, which can create a cycle that increases their fall risk.
8. Environmental Hazards:
Many falls are caused by environmental factors, such as slippery floors, uneven sidewalks, poor lighting, or cluttered living spaces. Older adults may not be as quick to notice or avoid these hazards, leading to a greater likelihood of falling.
9. Cognitive Decline:
Dementia or cognitive decline can impair a person’s ability to judge distances, remember to use assistive devices like walkers or canes, or recognize potential hazards. This can increase the risk of falls.
10. Dehydration and Nutritional Deficiencies:
Dehydration or deficiencies in important nutrients like vitamin D or calcium can affect balance, muscle function, and bone health, making falls more likely.
In summary:
Falls in older adults are often the result of a combination of these factors. Addressing some of these, such as improving strength through exercise, addressing vision problems, or making environmental changes at home, can significantly reduce the risk of falls.
What can I do to Prevent a Fall?
1) Ensure your home is safe
As 70% of falls occur within the home, ensuring our home environment is safe is essential.
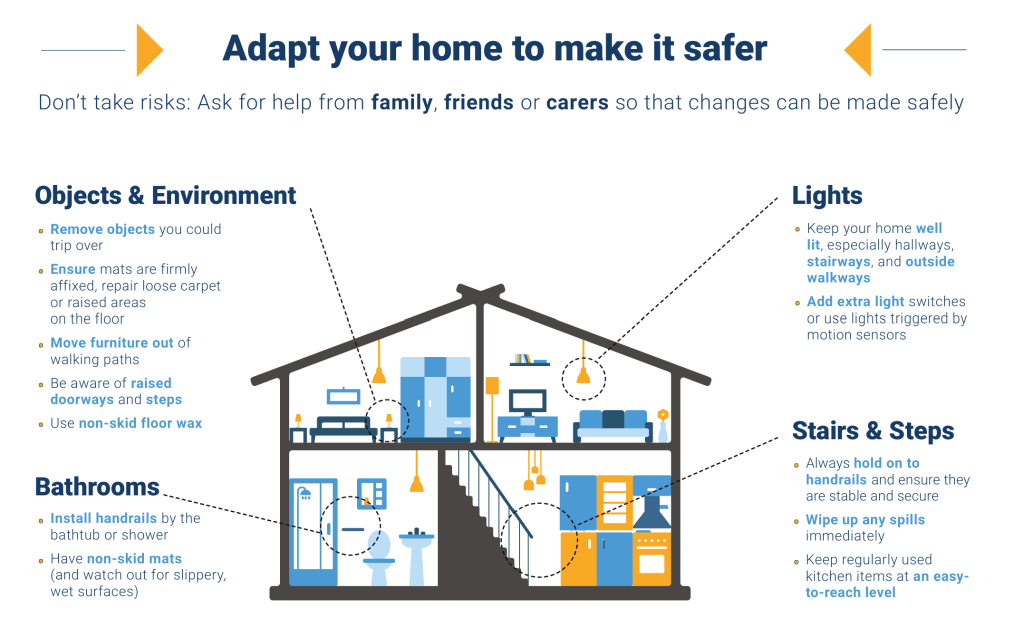
The following infographic suggests some ways you may adapt your home to make it safer.
If you are staying a HDB flat in Singapore, you may be eligible for government subsidised home modifications under the HDB EASE programme. This includes installation of grab bars and shower chair, installation of ramps and lowering of kerbs, and application of slip-resistant chemical treatment to tile flooring.

Refer to the HDB EASE website for more details.
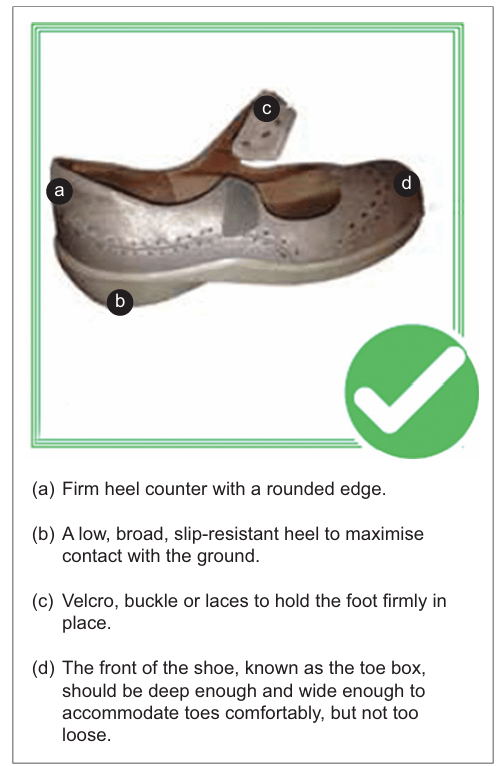
2) Wear appropriate footwear
Footwear can cause falls if it doesn’t fit well, is slippery, or doesn’t support the feet properly. Shoes that are too loose or tight can make walking harder and lead to tripping. High heels can make you unsteady and more likely to fall. Shoes with slippery soles or no grip can cause slipping, especially on smooth or wet floors. Flip-flops and backless shoes don’t stay on well, making it easy to trip. Wearing the wrong shoes for activities, like walking in sandals on rough ground, also increases risks.
To avoid falls, wear well-fitting shoes with good grip and support.
3) Know your medication
Medications can increase fall risk by causing dizziness, low blood pressure (orthostatic hypotension), muscle weakness, or impaired cognition. Drugs like sedatives, antidepressants, antihypertensives, and opioids may lead to drowsiness, confusion, or slower reflexes, while others, such as antihistamines, can blur vision. Polypharmacy (using multiple medications) can amplify these effects.
To reduce risks, regularly review medications with a doctor, monitor for side effects, and avoid unnecessary drugs. Stay hydrated and rise slowly to prevent dizziness. Common culprits include sleeping pills, blood pressure medications, and painkillers.

4) Check your vision regularly
Poor vision can make it harder to see obstacles, uneven ground, or judge distances, leading to falls. Trouble judging steps or objects might cause tripping. Limited side vision can make it hard to notice things nearby. Blurry vision or eye problems like cataracts can hide dangers, and bright lights or darkness can make moving safely difficult. Seeing double or slow eye movements can also affect balance. Moving between light and dark areas can be confusing.
To stay safe, get regular eye check-ups, wear the right glasses, use good lighting, and keep spaces clear of clutter.
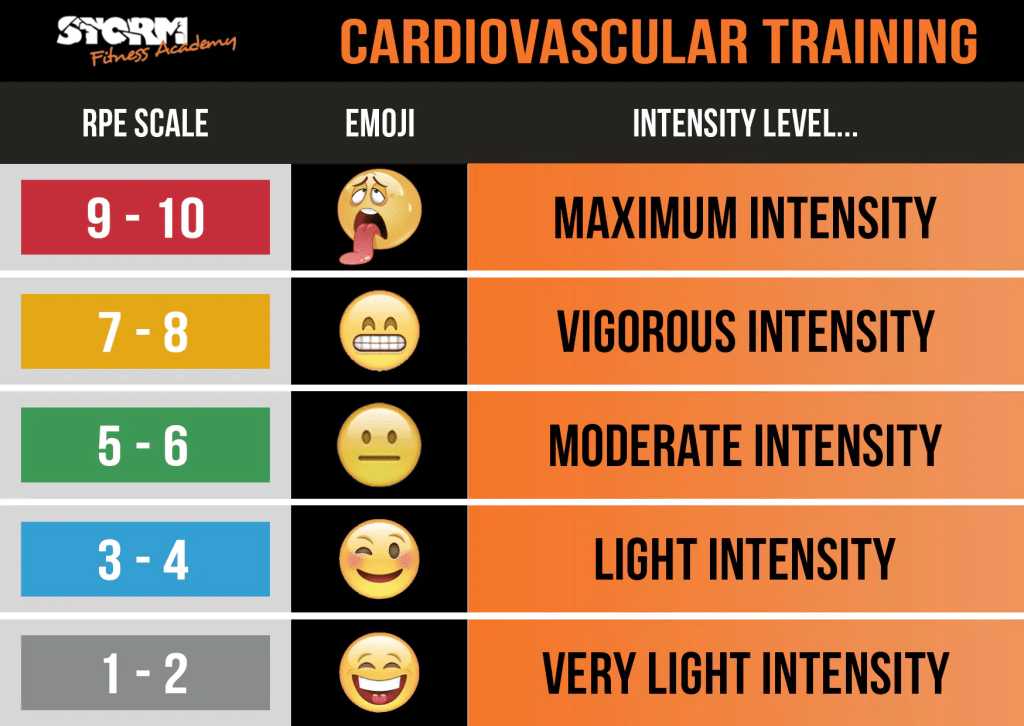
5) Engage in regular strength and balance exercises
Strength and balance training helps prevent falls by making your muscles stronger and improving your ability to stay steady. Stronger legs help you stand, walk, and climb stairs more safely. Better balance helps you avoid tripping or stumbling. Regular strength and balance training teaches your body to react quickly if you lose your balance, so you are less likely to fall.
Some examples of balance exercises include standing on one leg, walking heel-to-toe, walking sideways and backwards. For best benefit, you should feel slightly unsteady while doing the exercises but not as though you are about to fall. Perform these exercises near a stable support for safety but avoid relying on hand support.
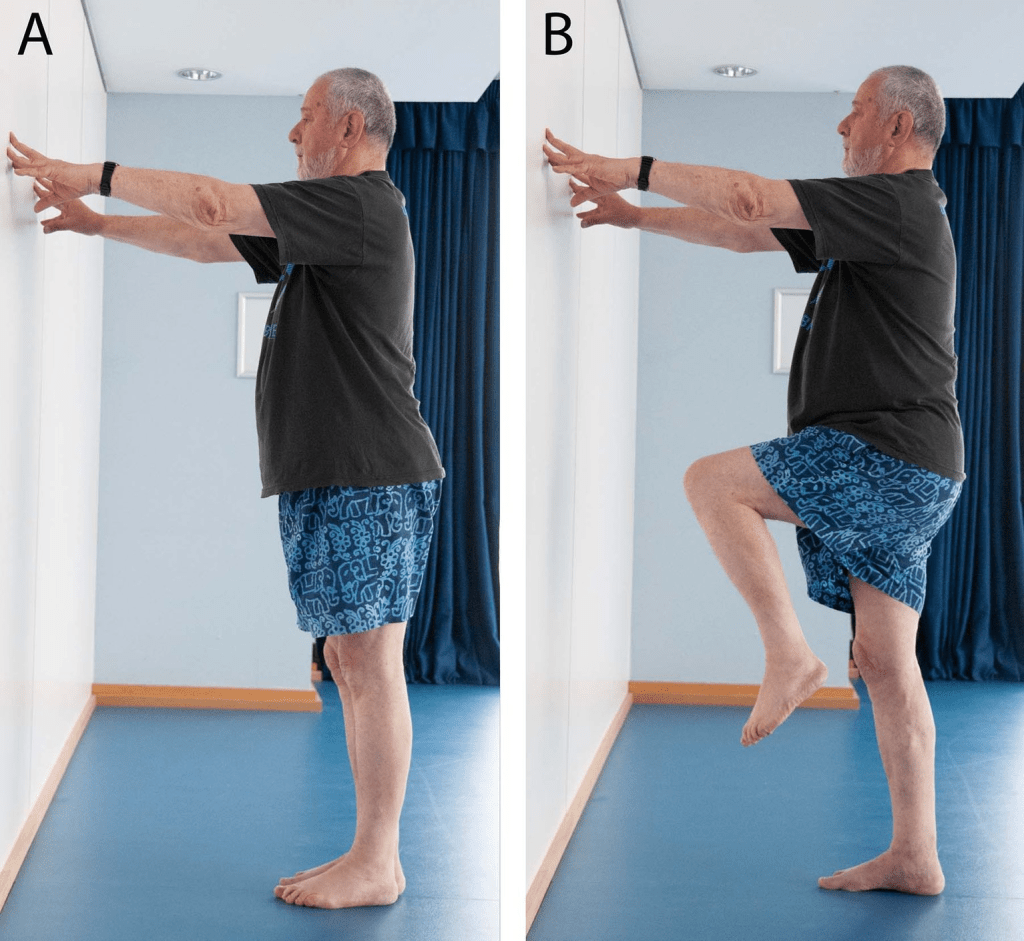
Standing on one leg
Stand near a wall with your feet slightly apart. Hold lightly onto the wall if you need to. Lift up one leg, keep your supporting knee soft.
Aim to hold for 10 seconds. Repeat 10 times on each side.

Heel-Toe walk
Stand near a wall with your feet hip width apart. Place one foot directly in front of the other, landing with your heel first then toe. Avoid locking your knees as you take 10 steps forward.
Repeat 3 times.
Source: https://www.nhs.uk/live-well/exercise/balance-exercises/
Doing these exercises 3 times a week helps your body stay steady and strong, keeping you safer in your daily life.
For a more customised strength and balance programme, Contact Us to arrange an appointment.